Pain: Why does it hurt and how does massage help?
Everything we do in life is to avoid pain and seek pleasure. Sometimes these signals get a little confused or a little overworked and therefore become accustomed to signalling pain. Then, they just won’t shut up.
This blog attempts to explain pain a little more easily.
There are two parts to this blog:
Part 1 - Looks at pain, how it is set up and why it persists.
Part 2 - Find out some steps to aid in your recovery.
DISCLAIMER:
This blog post is aimed at providing you with a better understanding of pain. It is by no means written to replace any care that you are currently receiving.
Pain referenced here is in regards to soft tissue pain. If you are in chronic (long-term) pain, seeking the advice of a health care professional is strongly advised.
Part 1 - Pain
Overview of pain:
Pain tells us that we are not in homeostasis, the balance of all the body’s systems and mind.
The sensation of pain is actually interpreted by the brain. If the brain perceives something as a threat then it responds to that sensory input as pain. This is why you can injure yourself and not have any pain until you look at it!
Feeling pain is the bodies way to protect itself. It is not a measure of the condition of the tissues.
It is important that you remember this as you read on.
Pain is usually felt with hard and fast changes to the bodies tissues. Gradual changes (such as posture) may not be perceived as a threat, initially, or until those tissues become over exerted (such as ligament or tendon strain due to repetitive misuse).
We all roughly have the same pain threshold (perception of pain at a certain level of intensity), but it's our tolerance to pain that varies.
Pain tolerance can be genetic, it can also be experience based, related to our perception of the pain and our own ways of coping.
Pains role:
Your brain interprets sensations and understands them as threat or not threat. Pain is designed to protect you.
The good thing about pain is that it changes our behaviour. It promotes learning to avoid further injury and it helps set limits on activity so that we can recover appropriately.
It causes you to be careful and adapt to using the body part differently or all together. If something is painful we limit that movement to avoid pain.
This is good in the initial stages of injury but eventually movement must return or pain will persist (more on this in the recovery section, part 2).
How pain works:
There are many little nerve sensors in our tissues (muscle, bone, skin, joints) that switch on when we experience different sensations. Sensations such as temperature, vibration, stretch, pressure etc.
Our skin has many of these sensors and different parts of our brain are dedicated to these different areas, and because a particular part of our skin gets more attention (like our hands) a bigger area of the brain is given to it. This can explain why some areas are more sensitive and hyper aware.
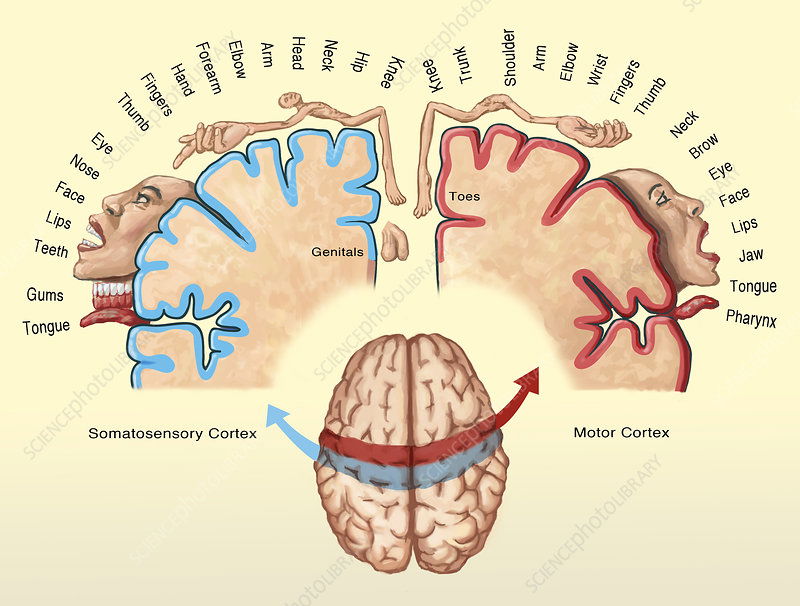 This disturbing image is a brain hormunculus. It's a way of depicting how different parts of our brain are dedicated to our body. See how the hands and face are grossly enlarged, that means more brain function is given to those parts (i.e. more nerve endings).So, these nerve sensors basically just tell the brain “who” is calling and “where” (e.g.pressure in the joint).
This disturbing image is a brain hormunculus. It's a way of depicting how different parts of our brain are dedicated to our body. See how the hands and face are grossly enlarged, that means more brain function is given to those parts (i.e. more nerve endings).So, these nerve sensors basically just tell the brain “who” is calling and “where” (e.g.pressure in the joint).
Nerve sensors are fast acting because they have a special myelinated sheath around them that helps transmit the signal quickly.
A sensation will activate the particular sensor and it will record the frequency of that sensation (strength, duration, pattern). The greater the frequency the stronger the stimulus.
Most sensors adapt to sensation, becoming less sensitive. Like when you jump into the sea and it’s cold at first but eventually you “warm up to it”.
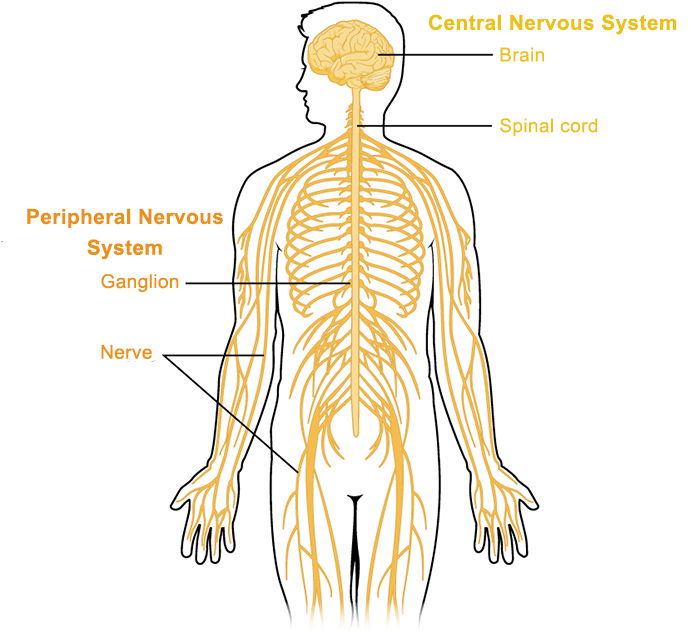 Peripheral nerves. These nerves send and receive information. The messengers (sensory nerves) travel to the brain and spinal cord. The nerves traveling to our body parts are motor nerves, they give us an action. Like spasm a muscle if it's been put on a hard and fast stretch.
Peripheral nerves. These nerves send and receive information. The messengers (sensory nerves) travel to the brain and spinal cord. The nerves traveling to our body parts are motor nerves, they give us an action. Like spasm a muscle if it's been put on a hard and fast stretch.
If a stimulus is perceived as particularly strong a different type of sensor will activate; a nociceptor (No-SEE-septor). These nerves elicit a pain signal.
Because they do not have the myelinated sheath around them they travel a bit slower, which is why when you cut a finger you’ll get a sharp, prickly sensation from the first type of sensor followed by the ache or burning sensation of pain by the nociceptor a bit later.
Slow pain signals? That brings me to a little aside: There is a thing called pain-gate-theory. Where if you’re experiencing pain touching another area lightly and nicely (or maybe even firmly) will potentially override your pain sensation. This happens because all those myelinated sensors travel faster than pain sensors so your brain interprets them first. |
Well, unless you focus on the pain.
Don’t think about the pain!
Injury and pain:
When we injure ourselves there is damage to the tissues and our immune system rushes to fix it. Our body creates an inflammatory response in order to heal.
I won’t get into this in huge detail (I think this post is getting painfully big as it is) but with the inflammation response we get certain chemicals at the site of injury: histamine and prostaglandins among others.
These chemicals sensitise the area, making the pain response more severe.
The immune system can actually be excited by stress. When we’re stressed cortisol and adrenaline trigger an immune response, this in turn signals the brain, the brain activates the cortisol system…and there we have a cycle.
Stress and pain:
Cortisol is a hormone we produce for different reasons, one reason is stress. Cortisol gets a bad rap but it is a protector. When we’re challenged it slows down body processes not necessary for you at the time, like digesting food and healing.
Cortisol can be linked to poor healing, loss of memory, loss of libido, depression, decline in physical performance (stress response!).
Cortisol does decrease pain (for the short term). In the morning cortisol is usually increased, rises a bit at lunch then declines again, hence why pain might be worse at night.
However, if we are in a long term stress response (dis-stress) and experiencing pain, that pain is only heightened and preserved through cortisol and our poor mental state.
| Long-term stress and pain usually leads to altered activity which leads to more inflammatory chemicals (which means more sensitivity!). |
Persistant pain
When pain persists past the tissues natural healing time frame it is more than likely that nothing is wrong with the tissues but that the area has become hyper sensitive and accustomed to pain.
The danger messenger nerves used to sending pain and the brain is so used to pain in that area that any stimuli, even minor touch, can be painful.
Usually with an injury there is a mixture of stress and thoughts that heightens the pain. Stress by its very design makes us more sensitive and if the injury or body part has emotional trauma linked to it (car accident, loss of job, loss of sport, loss of independence, assault) then any stimulus to that area is going to hurt. A lot.
Then I’m doomed? DOOOOMED!
Not at all. Persistent pain doesn’t have to persist forever (in most cases). Remember when I said earlier that pain is not a measure of your bodies condition?
It is a stimulus response to avoid any further danger.
Yet, it is the fear, caused or coupled by stress and emotion and lack of understanding, that makes our pain worse and persist. Fear of not knowing what’s going on in our bodies. Fear of losing a job. Fear of not playing sport. Fear of surgery, therapy. Fear of re-injuring.
Fear creates tension. Tension creates pain. Pain creates fear.
(Oh, look, another positive feedback loop)
If you’ve had an injury and have been told that there is nothing wrong you might be pretty pissed because you’re feeling pain and someone told you that you shouldn’t be.
Your pain is very real. Yet, it is most likely not a result of that injury anymore.
Knowing this is very vital as it will enable you to start getting better. As you start managing your pain and recovering you will be able to move more and do more because when you think you feel pain you can stop the fear and tell yourself: “no there is nothing wrong”.
Eventually, with coping strategies discussed further, you can begin to shut down that pain pathway!
Part 2 - Recovery
Pacing, patience and persistence = recovery
It is important to note that pain saps us of energy because the body is trying to heal. When dealing with ongoing pain you must be kind to yourself.
Yes, with pain you must initially limit your activity or a certain movement in order to minimise pain and prevent re-injury. However, when we stop a particular movement we generally start compensating. Sometimes this compensation becomes painful so we stop doing that.
Before long we’re not moving at all and experiencing pain everywhere.
It is important that you keep moving!
Not moving only makes us stiffer. Stiffness puts minute strain on our bodies. And minute strain on an already sensitised body can increase pain.
For those who have healed from an injury but still experience pain, reminding ourselves that the pain is not a measure to our tissues condition can help you to overcome this pain.
Remember: Recurrence of pain does not mean re-injury.
Some cue has been set off to activate the virtual representation of the old injury (the part of your brain that identifies that body part with that old pain).
This is a flare up. A flare up is that increase in pain, often sudden, that leaves you debilitated for hours or days. Flare ups can be delayed by a day or so.
Steps to an active recovery
Find your baseline
The amount of activity that you can do and know that pain won’t flare-up.
Start your recovery with a little bit and slowly progress. If you know you can walk for only 15minutes before you experience pain, start with 10minutes. Then progress to 15 after a week or so.
Plan your progression
You could plan on increasing your walk each day by one extra minute. Don’t break the plan and push on. You must be patient otherwise you can bust your progress and feel worse for it.
Don’t freak out at flare ups.
They’re inevitable as you figure out what you can do. But remember, it’s just an over reactive response from your nervous system.
A flare up is just your nervous system aiming to protect you.
Remember, it’s a lifestyle!
In the short term you’ll be planning a lot. You benefit from trying the happy activities.
Challenge yourself a little more when you start to become more confident.
Your virtual body:
Recall when I said there is a part of our brain that is connected to every part of our body? That creepy hormunculus thing? Well, when we imagine a movement we’re pre-planning it in the bit of our brain that is associated with that part of the body.
This is your virtual body.
| When pain pathways have been set up for so long they become almost habit. Your brain, the part of it that is linked to that specific site of injury, is on standby mode. So every time you do something that may just be a little bit threatening, like a sudden turn or jolt, the brain immediately goes into threat mode and reminds us of pain in that area. |
Access your virtual body by visualising yourself doing the movement that causes you pain. Visualisation is a powerful tool we often don’t implement. A lot of athletes do this, so we should as well.
If you know that bending over hurts, then visualise yourself doing the movement and it not hurting.
Visualise yourself doing the movement easily, fluidly and in a controlled manner.
Visualise yourself being happy about doing the movement. Being relieved by the movement. Visualise the movement then perform the movement.
Move gently, easily and just a little bit. Move with an out breath. Don't push yourself into a pain response.
Remember: this is only with chronic pain and not immediate injuries.
Massage and persistent pain:
You all know what I’m going to say…Massage is great for managing long term pain!
But how?
- Massage helps calm your body. By calming the body you calm the mind.
A lot of the time, with on-going pain, our nervous system is hyper-aware. A relaxation massage helps to calm down the hyper-aware and hypersensitive signals. - Because massage can be varied in techniques and pressure it can be suited to the individual and their level of discomfort.
- Trigger points establish themselves for various reasons but if you’ve ever had trauma to your body you’re more than likely going to have trigger points. Massage is great at working out these achey little beggars.
- Massage therapy looks not only at your sites of pain but also at other imbalances that may have resulted from your injury or pain.
- Massage works with the soft tissues and the nervous system simultaneously, thus helping to send different and positive “tunes” to the body and switch off pain signals!
| Neuromuscular Therapy helps to slowly retrain your body through massage and gentle exercises so that faulty movement patterns that may be putting strain on your muscles and joints can be corrected. |
Self care for pain and recovery:
There are many other things you can do to help manage your own pain.
- Meditation and breathing exercises. By controlling your breath and calming the mind you will help yourself to reduce stress, and remember a stress response does hype up pain.
- Heat packs (not on immediate injuries) and gentle self massage with muscle rubs. Heat gets blood into tissues which can aid in healing, movement and will help with stretches.
- Ice can be soothing, especially with acute injuries. Put ice packs in damp cloths to avoid it sticking to your skin. Only ice for short periods of time. Ice constricts blood vessels and this means your tissues aren’t getting proper flushing, so only ice if you feel a big flare up happening after a lot of activity.
- Get some sleep! Sleep is paramount to healing. Without decent sleep you cannot heal properly.
- Try different ways of exercising. Swimming is a good one as water provides a subtle resistance but also helps alleviate gravity. Mix it up. If you have to do strengthen and rehab training one day, do a swim or something fun the next day.
- Eat a lot of high nutrient foods. Without proper nutrients how can your tissues function and heal properly?
- Do your prescribed stretching and exercises. These may have been given to you from your physiotherapist, massage therapist or other health care professional. They should be followed and maintained and check ups with them done to note your progress and advance to the next level.
- Keep a pain diary. It keeps you in track of your progression and will help link things together. You may notice when your mood is worse your pain is worse, for example.
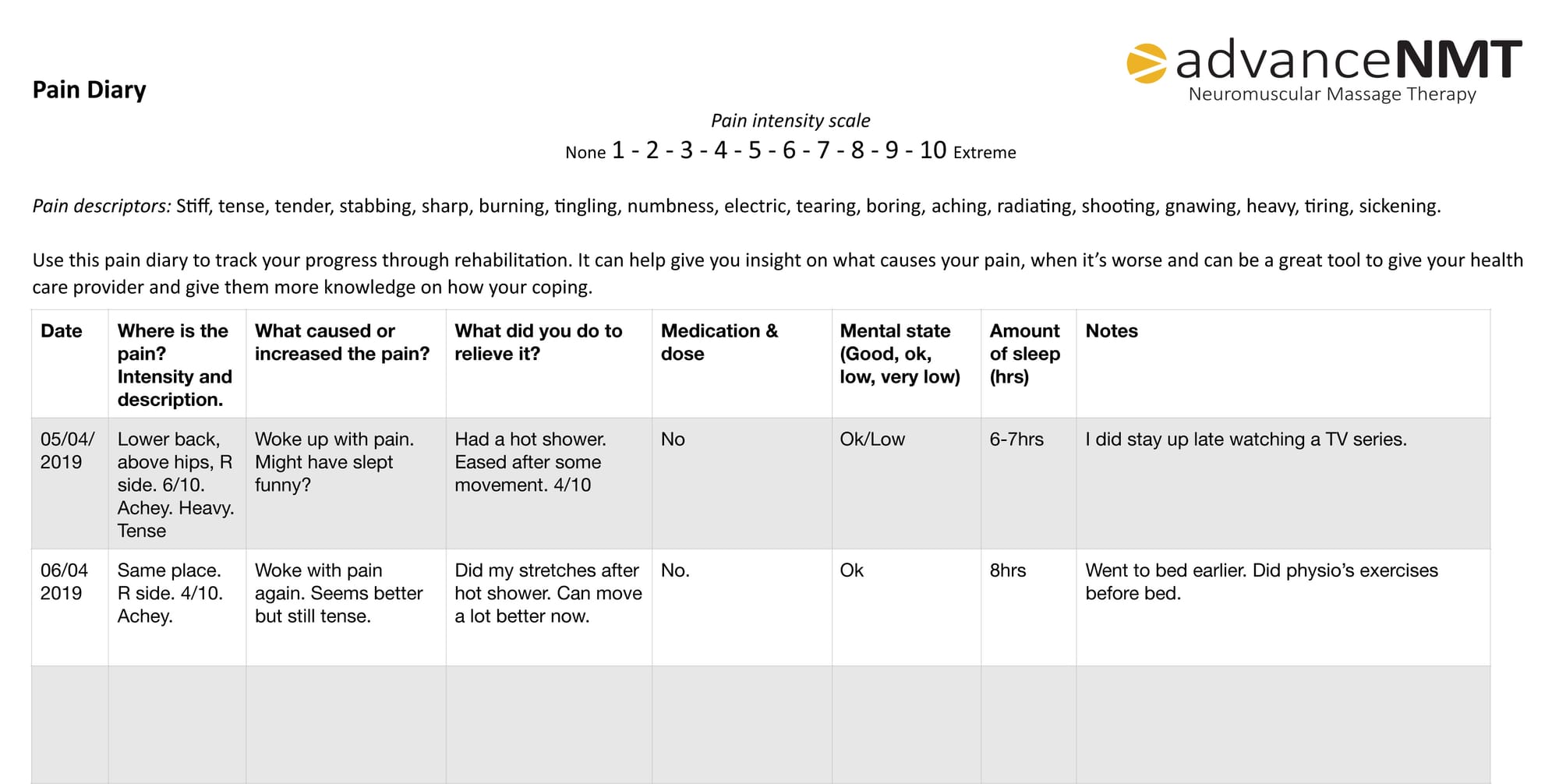 This is an example. Feel free to download the blank version below in either PDF, Word or Pages document.
This is an example. Feel free to download the blank version below in either PDF, Word or Pages document.
Pain Summary:
Once an injury has healed and pain remains it is normally not an indication that there is still anything wrong. Rather it is your brain that is used to receiving and perceiving a "threat" at that injure sight.
Couple this injury with fear (fear of losing a job, fear of not being able to play sport, fear of the unknown etc.) and the hypersensitivity of that previously injured site is exacerbated.
Yes, achey trigger points, muscle stiffness/shortness, and movement compensations may be present but these can feel much worse than they are for us, because our brain is used to playing the pain tune.
However, getting your movement correct and stopping any compensations to movement will aid in your recovery.
Remember:
Understand sometimes these things take time.
Managing and overcoming chronic pain takes action (correct action), actions require energy, energy requires recovery (sleep, nutrients, good mental state etc.)…all of this takes time!
Understand that set backs will occur, but you must not give up on your road to recovery.
Keep reminding yourself that your pain is a protective response. Flare ups will happen when you become more active. It is a protection response, as long as you have not re-injured yourself (e.g. a fall) your body is fine.
So be kind to yourself. Do not fear the pain and do not put too much pressure on yourself to be magically pain free within a few short days or weeks!
This information was derived from the following sources:
Butler, D., & Moseley, G. (2003). Explain pain (2nd ed.). Adelaide: Noigroup Publications.
Brukner, P., Clarsen, B., Cook, J., Crossley, K., Hutchinson, M., & McCrory, P. et al. (2017). Brukner & Khan's Clinical Sports Medicine (5th ed.). Sydney: McGraw-Hill Education Pty Ltd.